Functional Electrical Stimulation
A Special Report
Maintaining long term health with FES training
Physically disabled people are the least active group in society but make up around a fifth of Britain's population - almost 14 million people.
According to Sports England, disabled people are twice as likely to be inactive as able-bodied people and this creates a multitude of health challenges.
Fitness can reduce and the risk of health complications and illness are likely to increase.
In this Q&A we speak to Dr Derek Jones of Anatomical Concepts, to explore how to exercise paralysed limbs despite having experienced a spinal cord injury or other neurological condition (including stroke, MS, Transverse Myelitis and more) using Functional Electrical Stimulation.
How does FES Cycling work?
Whilst motorised bikes that can move paralysed legs with passive cycling are popular and they do help prevent joint contractures, the addition of FES ensures that exercise is active and this has a more powerful health benefit.
For example, various combinations of leg muscle groups - at least the quadriceps and hamstrings - can be activated in order to achieve an effective cycling action.
Each muscle group is "switched on" during only part of the 360 degree crank rotation, to ensure that stimulation of each group
results in a positive crank moment.
This is achieved by synchronising the delivery of muscle stimulation to the movement of the bike pedals.
An FES bike typically monitors the speed of the pedals and the effort generated by the user and uses this information to modulate the stimulation delivered to the muscles.
Products like the RehaMove system allow the user to set a target cycling speed and level of resistance to pedalling.
This allows the user to get stronger over time.
Most products are available in a form that will also allow upper limb exercise too and utilise the arm and shoulder muscles if these have been affected by the condition.
There is even a version that allows a person lying in bed and in intensive care to use FES Cycling and there are many benefits of this.

You mentioned using a stimulator with other functional exercise. How does this work?
Some clients will use the FES unit of the RehaMove system independently from the bike, with software called Sequence Mode, that allows other forms of exercise to be augmented with FES.
Instead of the stimulator reading data from the bike to know when to turn on or off the stimulation, we can set the unit to run on a sequence set by the number of seconds of stimulation of each channel, or programme a sequence to a manual button press.
For example, clients often use the RehaMove stimulator to aid in sit to stand work.
Usually the client would set up in a standing frame, then use a standing programme which would activate the quadriceps to get to standing, followed by a short activation of the glutes to add stability.
These would then turn off, followed by an activation of the hamstrings to allow a controlled return to the seated position.
This sequence can be set to run automatically on a loop, or with further control using a manual trigger press.
Clients find this to be very engaging and challenging to perform.
We can use this software in lots of ways including things link shoulder stabilisation, dorsiflexion, hand flection and torso stabilisation, and there are preset templates with the software.
We see therapists getting creative and integrating cable machines, bands, and other gym equipment for challenge.
Equally, using every day objects such as forks, cups etc to work on movements that help clients work towards feeding themselves or brushing their hair.
FES can really cover the bases of a device that can aid in every day functional health (cycling) and specific rehab goals (sequence mode).
How much electricity is being used?
The amount of electricity is very small.
Technically, the electrical waveform used will normally be a bipolar, rectangular pulse.
The maximum current will be around 130 mA.
The FES unit that makes the muscles contract delivers stimulation to the surface of the limbs via two surface electrodes placed on the limb segments with a gap between them.
The current flows in to the tissues via one electrode and out via the other one and in doing so, providing the amount of energy is sufficient, activates the nerves that bring about a muscle contraction.
There are other stimulation parameters to consider beyond current; namely pulse width and frequency.
The combination of current, frequency and pulse width can be varied by the FES unit to influence how strong the muscle contraction will be.
Some products will vary some of the parameters automatically within safe limits and of course allow the user to make changes.
Who can and cannot use FES Cycling or Sequence Mode Exercises?
Although most commonly practices by people with a spinal cord injury, FES Cycling is also used successfully in people with upper and or lower-limb dysfunction in a range of other neurological populations such as Stroke, MS, Transverse Myelitis and in children with cerebral palsy.
Just as with any medical product there are also contraindications and some cautions to using them.
These include things such as active fractures in the limbs being exercised, joint contractures that prevent a cycling action, pregnancy and the presence of certain types of implanted medical devices.
Contraindications will tend to vary over time and with developments of the technology but these should always be checked in each individual case.
When the upper limbs are to be exercised with FES it is important to verify the integrity of the shoulder joints.
When indicated, this exercise can be fine tuned to preserve shoulder function and prevent contractures in the upper limbs.

What does FES feel like?
Many of our clients have an injury which means they have little or no sensation in the area in which the electrodes are applied. So nothing is felt.
This doesn’t mean that you can make the stimulation as strong as possible as there are other things to consider.
For example, you need to be aware of skin irritation at the electrode sites and provoking muscle fatigue resulting in a
metabolic insult, by having the intensity of stimulation too high.
With some users who have sensation, the level of stimulation can be reduced to diminish any discomfort.
We have met some people who find it difficult to tolerate useful levels but this is quite unusual.
With some levels of injury, (above T6 level) care must be taken, especially at the beginning of use, to avoid autonomic dysreflexia.
Most people who might be susceptible to this condition will have learned to recognise how the onset of this feels at an earlier stage of rehabilitation.
If someone feels unwell when using a FES bike this should be halted immediately.
It's also good idea to ensure that bowel and bladder are clear before exercising.
What are the other benefits to FES Cycling and training?
A range of physiological benefits has been observed in clinical studies of subjects with spinal cord injuries, including improvements in cardiopulmonary fitness, muscle strength and bone density.
Sometimes FES Cycling helps to calm muscle spasms.
Stimulating the gluteal muscles during cycling can help reduce the risk of pressure ulcers and the stimulator can also be carefully used to assist with wound healing.
Of course there are also psychological benefits of exercise and regular activity.
Some clients also report that they feel positively about retaining / improving their muscle mass for aesthetic reasons.
Can you build muscle with electrical stimulation?
Regular training with a RehaMove system or other FES bike will definitely encourage growth of the leg muscles and fight off
muscle atrophy.
By varying the stimulation parameters, lower limb muscles can be conditioned for endurance or power.
Although the technology has improved over time, it is less efficient to trigger a muscle contraction using FES than it is for the body working "naturally".
The body has a much more efficient process for recruiting muscle fibres to contract.
It is unlikely that someone starting to use an FES bike for the first time will generate much power.
It takes time and patience - think - more of a marathon than a sprint.
Does electrical stimulation relax muscles?
Some users have troublesome spasms in the legs. These can be a nuisance and often medication is offered to try and reduce these.
Unfortunately, oral medication is not always effective, can make the patient drowsy or lose its effectiveness over time.
Some patients elect to use an implant which can deliver precise amounts of medication to manage the spasms.
An FES Cycling intervention can help a majority of persons to damp down their leg spasms.
Sometimes these get worse initially as the legs get stronger but in these cases the stimulation parameters can be fine tuned to help. Also stretching, and leg massage prior to a session can help.
How does someone get started with FES Cycling or training?
Functional electrical stimulation in general and FES Cycling in particular is a safe and widely used modality with a good evidence base for supporting long term health.
We would always encourage exploring the various options and thinking carefully about the possibilities.
The technology available from ourselves and other suppliers will fundamentally attempt to do similar things but with differences in the user interface.
Our approach to working with the RehaMove FES Cycling system asks potential clients to complete a short risk assessment.
Providing the client is safe and suitable to use FES, we ask a therapist to visit the client with a system to talk over their specific goals and give a full demonstration.
We then follow up with a report which details the discussions, the exercise programmes that were demonstrated, and a recommendation on how they may adopt the system into their routine.
In an ideal world, FES Cycling and FES Training would be utilised daily to simply help individuals stay active, reducing the risk of longer term ill health or complications.
With driven clients and therapist input it can also help improve targeted, rehabilitation outcomes.

Can you stimulate a denervated muscle?
The short answer is ‘Yes you can.’ And, you probably should.
A related question, of course, might be ‘why would you want to’ - we will get to that shortly.
Denervation of skeletal muscle can occur following a spinal cord injury affecting the low lumbar and sacral regions, or with peripheral nerve injuries.
The many nerves that fan out at the end of the spinal cord are known as the cauda equina, due to its appearance being likened to a horse's tail.
The spinal cord actually ends at the upper portion of the lumbar (lower back) spine but the individual nerve roots at the end of the spinal cord that provide motor and sensory function to the legs and the bladder still continue further along the spinal canal.
Damage to these by trauma, tumour, or other origin can cause many "red flag' problems including a flaccid type of paralysis.
Peripheral nerve injuries are commonly seen and can also be difficult and frustrating to manage.
These result from contusion, crushing, stretching or cutting of nerves such as the axillary nerve at the shoulder, the radial nerve in the arm, the ulnar nerve at the elbow, and so on.
The "traditional" approach to dealing with peripheral nerve injuries has tended to focus on limb positioning and the prevention of contractures through passive or stretching exercises.
What happens when a muscle is denervated?
Following an injury a denervated muscle alters its structure in many ways, and over time the normally excitable and contractable muscle fibre tissue is replaced with collagen and fat.
This tissue becomes less capable of contracting as this process takes shape.
The muscle atrophy and changes that rapidly follow denervation can make any intended rehabilitation process an
extremely difficult task.
If reinnervation is a possibility, this opportunity is lost without effective intervention.
Reinnervation cannot complete if the former muscle's structure is lost and no longer supports contraction.
As these effects progress, the loss of muscle bulk and tissue quality lead to a poor general trophic situation.
How do you deal with muscle atrophy?
Electrical stimulation can now be used to stimulate denervated muscles and to cause contractions that prevent or reverse atrophy, as well as possibly supporting the regeneration of peripheral nerves - if this is to be expected.
Once upon a time there was concern that using electrical stimulation could actually deter reinnervation but now evidence suggests that this should not be an issue.
The whole topic of using electrotherapy for denervation has been controversial over the years. It is a fact that forms of electrical stimulation have been used with denervated muscle since the
mid-1800's.
In 1962, "The Denervated Muscle", edited by Ernest Gutmann was published and this work is still not a bad place to start when you wish to learn about this phenomenon.
Gutmann and his collaborators were conducting research on long-term denervation of skeletal muscle beginning in the 1940's and his work is still widely cited even today.
Of course, this research was largely descriptive and what was possible was limited by the technology available at the time.
Even in the 1990's though, using electrical stimulation with cases of denervation has been controversial with fears that the level of intensity needed would lead to the potential
for skin burns. In our experience, providing good methods are followed, the risks are very low.
In Europe the multinational European RISE study and the work of Helmut Kern in Austria and many others has helped to change the minds of many on the safety and effectiveness of electrotherapy for denervation.
The RISE study used specially developed electrical stimulation equipment and showed that it could be used safely by clients at home who had complete denervation.
The equipment could be used to rescue the muscle tissue bulk and quality even with clients many years after their injury.
The researchers also developed protocols for application which guide our own practical work today.
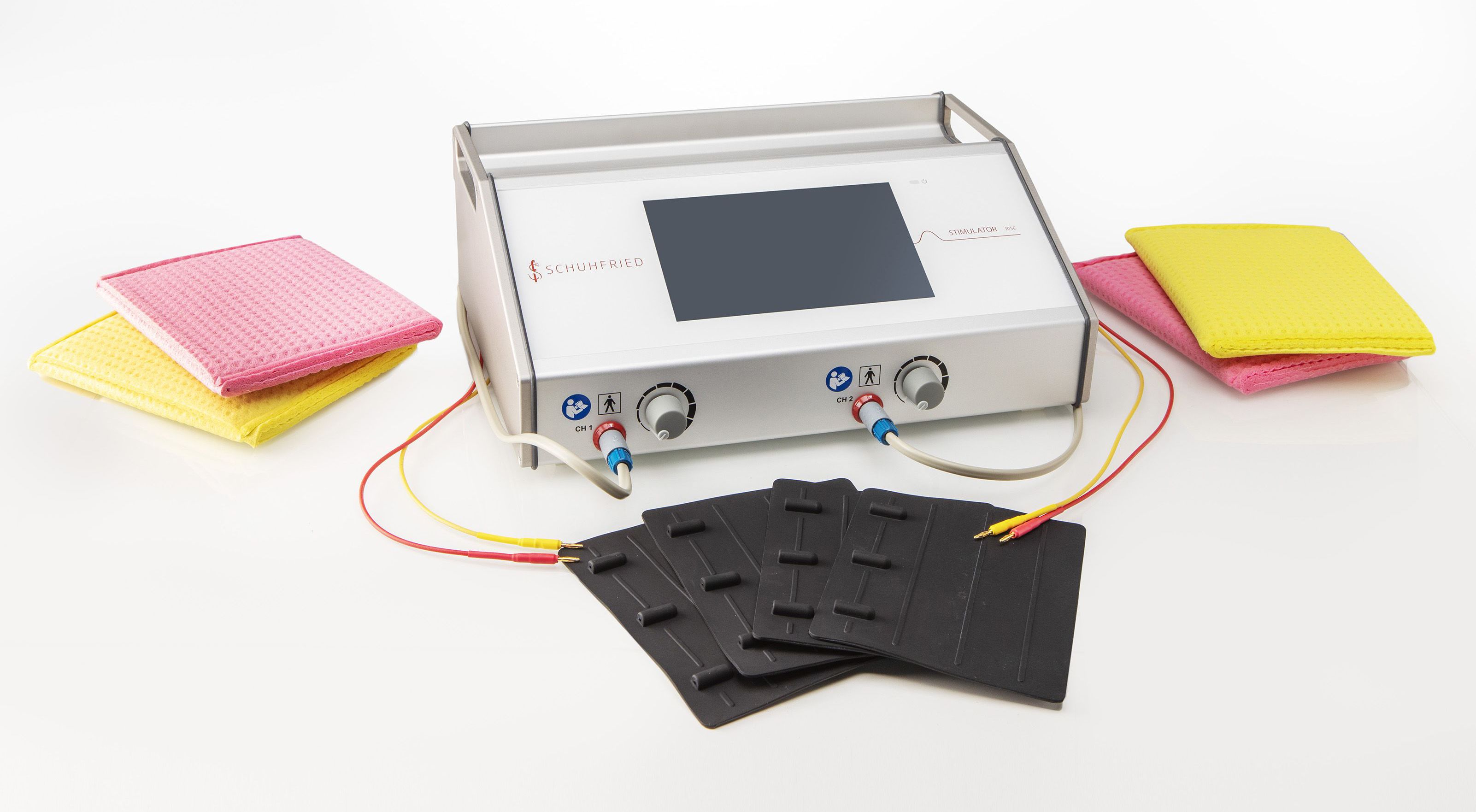
This study utilised the equipment which has evolved into the RISE stimulation unit we use today.

What stimulation parameters are needed?
The type of FES we see used with any of the FES bikes on the market such as the RehaMove 2, will not work with denervated muscle.
This is because the electrical energy delivered by these systems relies on the presence of intact motor nerves.
Muscle stimulators that rely on an intact nerve structure will typically deliver bipolar rectangular pulses with waveforms described by three parameters - frequency, pulsewidth and current.
You would expect to see these deliver pulses in the ranges 20 - 50 Hz (frequency), 0 - 130 mA (current) and 100 - 500 microseconds pulse width.
When the nerve structure is intact these parameters are sufficient to excite the muscle fibres to contract.
In contrast, the RISE Stimulator can still deliver a bipolar waveform but the stimulation parameters are very different.
We may use frequencies as low as 1 or 2 Hz, pulse widths of up to 200 milliseconds, and currents as high as 200 mA.
With spinal cord injuries resulting in a flaccid paralysis of the legs we would today use large electrodes (either specially designed safety electrodes or wet sponge bags with carbon rubber) that cover as much muscle tissue as possible.
This is because the aim is to make the muscle fibres contract directly, rather than rely on the (absent) nerve structure that would typically be used by commonly available electrical stimulation units.
Two protocols are typically used - one that is low frequency and seems to induce a twitch in the muscle and a second protocol that produces a tetanic contraction.
The first protocol encourages a normalisation of the muscle structure, and the second protocol strengthens what has been recovered.
Therapy Progression
In starting to use this equipment it is possible that a twitch contraction can be elicited but not a tetanic one.
Period testing can be used to verify when a tetanic contraction can be generated and a feature is built into the RISE unit to allow this.
Clients will generally have to use the unit 5 or 6 days a week at the beginning.
As therapy progresses to use tetanic contractions these can produce leg extensions and ankle weights can be utilised for resistance if desired.
With peripheral nerve injuries we can quite often find that we have muscles with preserved innervation alongside denervated ones.
We then do not want to overload the normally innervated muscles.
The fact that the paralysed muscle has lost its normal accommodation ability allows for selective stimulation of denervated muscles.
We do this by changing the waveform shape to a long exponential (triangular) pulse rather than a rectangular one.
We can therefore achieve selective contraction of the paralysed muscles.
Specialist equipment
There are a number of hand-held units on the market that in general terms can generate the parameters suitable to elicit a denervated muscle to contract.
However, these rarely generate the current intensity or range of parameters necessary to cover all applications.
Typically these units are okay with smaller upper limb muscles but not adequate when dealing with quadriceps, gluteal and other larger muscles.
The RISE use has two channels and is very simple to use. The unit can have the settings fine tuned via an easy to use interface and then the unit can be placed in a "home user" mode which prevents accidental changes to stimulation parameters.
The user need only then understand how to secure the electrodes and rotate a control knob to set the stimulation intensity.
As outlined earlier, consistency is key to producing effective results, and the user will need to commit to a regular schedule to see the benefit although this can be reduced once a strong foundation has been established.
You Can. You Should. Here is Why.
One of the real drivers for clients to use electrical stimulation has been the resulting appearance of their legs.
Stimulation builds muscle, and this has aesthetic benefits that users care about.
Denervated stimulation can support the user to add 3 to 5 cm of muscle girth to their thighs.
Clients (or therapists) should be encouraged to take measurements at regular intervals to provide markers for progress, and provide motivation to continue with therapy.
It is also important to remember that developing muscle bulk and quality reduces pressure ulcer risk and improves local circulation.
Anatomical Concepts have extensive experience working with & training both clients and therapists in the stimulation of denervated muscle.
Following a short risk assessment they can offer client demos anywhere in the UK, and regularly provide onsite or remote clinical training in the practicalities and expectations of working with the RISE stimulator.
For those seeking support with neuropathic or nociceptive pain, they also provide support and guidance on using the Stimulette Edition5 S2X.
Find out more about Anatomical Concepts at anatomicalconcepts.com

L300 Go: The stimulating and stabilising drop foot solution
Amy McColm is an Orthotist and Academy Clinician at Ottobock - a world-leading manufacturer of prosthetic limbs, wheelchairs and orthotic supports.
The company is a worldwide distributor of the FES device, the L300 Go.
The hugely popular drop foot stimulator works by delivering a charge through the nerve and the belly of the muscle, making it contract so the leg can move more naturally.
The device has improved quality of life for countless patients across the globe, from stroke survivors to Parkinson’s and multiple sclerosis patients.
Amy says: “The L300 Go massively reduces their risk of trips and falls, enabling many people to walk independently.
“We've seen incredible results for patients who don’t have to rely on walking sticks anymore. This can massively increase their confidence.”
The wireless device is strapped around the calf, with a single electrode that clips into the cuff, and up to two channel stimulation delivering a charge.
This design eliminates the need for a foot switch, making the L300 Go lightweight, comfortable and easy to use.
Every time it's set up, it's completely individual. And everyone will have a different tolerance threshold, and a different muscle contraction threshold. So it's set up for each individual user
“Standard orthotics and AFOs have their place, but patients often find these bulky and heavy, and you have to be able to fit a shoe over the top.
“While a standard solid ankle AFO will hold the ankle in one position, the L300 Go supports movement, which can lead to improved range of motion at the ankle.”
The L300 Go can be tailored to the individual’s needs, with settings altered throughout the day and through the course of rehabilitation.
The clinician will assess the patient to set the level of intensity required to get the muscle to contract.
They can then alter how rapidly the charge is triggered, tailored to the patient’s walking pattern.
The device also offers a training mode, again programmed to the patient’s requirements.
Amy says: “Instead of passively stretching the foot, the patient can sit down for 30 minutes with the L300 Go lifting their foot for a set number of seconds, and then a period of rest, repeating until the end of the program.
“The physios can tailor that to the patient’s needs. It can be very specific.
“Every time it's set up, it's completely individual. And everyone will have a different tolerance threshold, and a different muscle contraction threshold. So it's set up for each individual user.”
“So all of that is reallyspecific to each users requirements..”
The L300 has evolved considerably over the years, with Amy and the wider Ottobock team continually looking at ways to improve it.
One recent addition is the thigh cuff.
This is used on the upper leg to control the bending or straightening of the knee and can be paired with the lower leg cuff or used as a standalone.
A mobile app allows gives patients control of the output, allowing them to slightly increase or decrease the intensity.
“If we set the level of intensity in clinic, there is a small amount of adjustment for the user to change throughout the day depending on the need or fatigue level.”
This is particularly useful for things like MS, where the patient may get tired throughout the day.

The app can also measure activity, such as the number of steps taken, allowing the wearer to track their progress.
This innovation has become increasingly in-demand across the rehab space, as patients become more tech-savvy and engaged with their rehab.
Amy says: “People want to be able to control their own rehab.
“You've had a lot of the control taken away from you. It's nice to be able to give some of that back.
“As technology is improving, mobile apps are becoming more and more useful.
“We are continually doing research and development to improve the product.
"We work closely with the manufacturers and have a community of experts to talk through any challenges.
“Customer feedback is really important too.
We have a global community helping us to shape the product.”
Learn more about the L300 Go at
Ottobock.com
Odstock Medical Limited (OML) - FES pioneer
Functional Electrical Stimulation (FES) uses small electrical impulses to stimulate muscles weakened by damage to the brain or spinal cord in adults and children.
The technique is used to assist walking, improve hand and arm function and assist other bodily functions.
Odstock Medical Limited (OML) is a major innovator of FES in the UK. Based at Salisbury District Hospital, the company provides clinical services, equipment and training.
OML is also researching into new applications of FES, for example, FES to reduce the some symptoms of Parkinson’s disease, improving the recovery after total hip replacement and the treatment of constipation in neurogenic bowel conditions.
Paul Taylor is co-founder and clinical director at OML.
A biomechanical engineer by background, Paul’s journey with OML began in 1986, with funding from the Department of Health to investigate electrical stimulation for the rehab of spinal cord injury.
“FES isn't a new thing. The concept goes back to the early ‘60s but it failed to make it into service back then,” Paul says.
“I designed a new kit, worked out clinical methods for using it and provided courses for teaching other people how to use it.
“We made a device specifically for stroke patients that was shown to improve walking.
“More patients got referred, more devices were made and it soon became clear that more and more conditions could benefit from FES.”
Despite promising research and routine use of FES in the former Yugoslavia, globally, the technique was slow to take off.
Paul and his team were one of the first to bring the FES into the clinic in the UK, with the aim of making it a routine application for patients at Salisbury and further afield.
While early investigations explored FES for spinal cord injury, it soon became clear that people with stroke and MS could find
significant benefit.
Paul explains: “We originally investigated FES to provide standing for people with spinal cord injury.
"If the equipment stopped working, they would muddle through and get around to telling you at some point.
“But if the walking stimulator for drop foot stopped working, the patients would be banging the door, wanting it replaced as soon as possible because it made such a huge difference.”
“This certainly shows that patients experience improved quality of life and improved activities of daily living.
“And for some, it's the difference between walking and not walking at all, so it does make a big difference.
“It's not one-solution-fits-all. We have a suite of solutions to suit individual patients for their individual needs.
“Likewise, we can use FES to improve knee and hip movement.”
NICE guidance from 2009 established FES as routine NHS treatment for drop foot due to brain or spinal cord injury.
Also, national guidelines for how FES is implemented in clinical practice have recently been published by the Association of Charted Physiotherapist In Neurology.
To access NHS treatment, patients have to be referred by a GP, MS nurse or neurologist.
But whether NHS or privately-funded, FES has been shown to be a long-term cost-effective treatment.
Paul says: “The latest independent study showed that FES is cost-effective in comparison to ankle foot orthoses (AFOs).
“Although the orthoses were cheaper, the adherence rate for FES was about double that of the AFO, and the improvements and quality of life benefits were greater overall.
“In fact, one of the patients from our original randomised controlled trial is still using their FES device 30 years later.”
OML’s technologies are now helping countless patients across stroke, brain injury, cerebral palsy, Parkinson’s disease and beyond, with new innovations currently under development.
Paul says: “We're developing a new stimulator device to give hand movement to people with tetraplegia. It's called Tetra Grip.
“We are also waiting to hear if we’ll get further funding to develop a new generation of stimulator, designed to extend the range of disabilities that can be helped by FES."
Despite significant evidence for FES, there are still areas of the country where it is not routinely funded by the NHS.
This year the MS society has launched a campaign to improve access to FES.
You can join their campaign at
www.mssociety.org.uk/care-and-support/professionals/evidence-professionals
Find out more about OML at
odstockmedical.com

